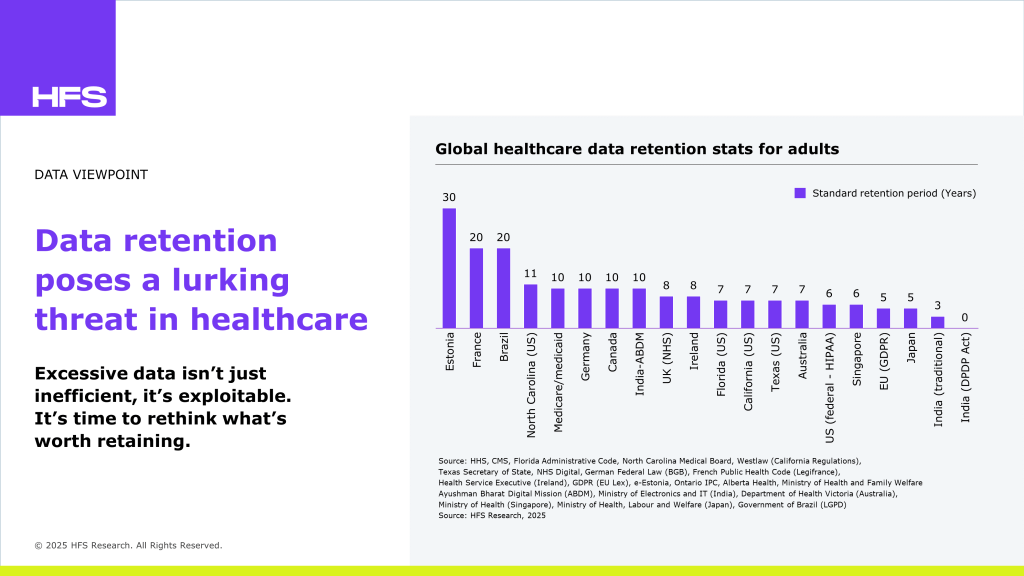
A comparative analysis of retention mandates across different global regions reveals a clear trend: Most healthcare systems store data for 7–10+ years, even as over 90% of that data goes unused for clinical care.
The result? An ever-expanding attack surface, inflated storage costs, and diminishing returns on digital investment. New privacy laws, such as the EU’s General Data Protection Regulation (GDPR) and India’s Digital Personal Data Protection (DPDP) Act, promote data minimization and purpose-bound storage. At the same time, decentralized models such as Estonia’s federated architecture and India’s Ayushman Bharat Digital Mission (ABDM) are shifting the focus of control toward patients. However, while ABDM enables long-term digital access to health records, it does not mandate deletion, creating a risk of indefinite storage unless DPDP’s data lifecycle mandates are actively enforced. Some of the key trends emerging from our comparison of data retention rules across regions include:
Enterprise healthcare leaders can’t afford to defend everything forever. By aligning legal, IT, and clinical operations around risk-tiered data retention and embracing federated, purpose-bound access models, they can dramatically reduce the attack surface, improve compliance, and lower breach impact. The future isn’t just about protecting more; it’s about storing less and being smarter.
Register now for immediate access of HFS' research, data and forward looking trends.
Get StartedIf you don't have an account, Register here |
Register now for immediate access of HFS' research, data and forward looking trends.
Get Started