This playbook is for health plan CIOs with one or more core administrative processing systems (CAPS). It embraces the key tenets of Services-as-Software™ (SaS) and leverages AI to reduce costs and operational risks.
This playbook’s approach should yield a 5% to 10% savings in operational costs while maintaining compliance and risk posture, depending on the types of outcomes.
HFS Operational Playbooks are practical guides to solving key enterprise challenges that consume significant costs, time, and resources. The playbook provides enterprise leaders a realistic roadmap with specific
“to-dos” to address their everyday challenges so they can clear mental and financial space to deliver next-level value.
The Big Beautiful Bill Act of 2025, the expiry of Affordable Care Act (ACA) subsidies, and Medicare sequestration will reduce government healthcare funding by about 10% annually, yielding a material reduction in revenues for health plans serving Medicaid, Medicare, and the exchange markets. It will exacerbate declining margins, elevating the priority of cost management. Medical management will remain the largest cost component, but technology costs, at two to three percent of annual revenue, can be material for a business running at sub-one-percent operating margins.
This playbook is for health plan CIOs with one or more core administrative processing systems (CAPS). It embraces the key tenets of Services-as-Software™ (SaS) and leverages AI to reduce costs and operational risks.
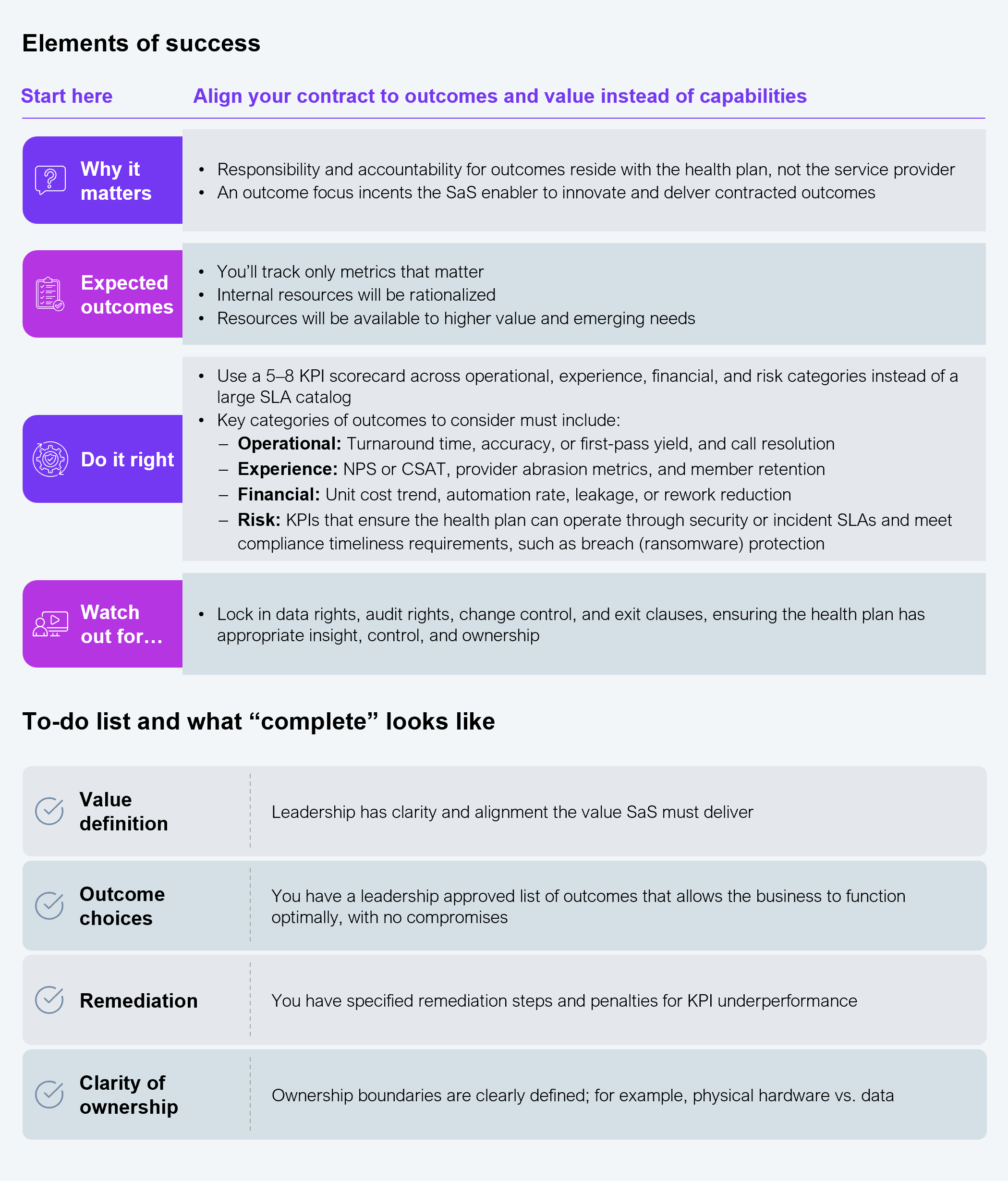
SaS (see Exhibit 1) will enable the move away from people-based delivery to IP-led delivery (AI-enabled risk stratification model), from capability or process outsourcing to outcomes orchestration (low provider call volume), and, crucially, from static annual agreements to contract-based, telemetry-driven value realization (prior auth leakage reduction measured by fewer avoidable calls, faster approvals, lower abrasion). The operational approach in this playbook should yield 5% to 10% in operational cost savings while maintaining compliance and risk posture, depending on the types of outcomes.
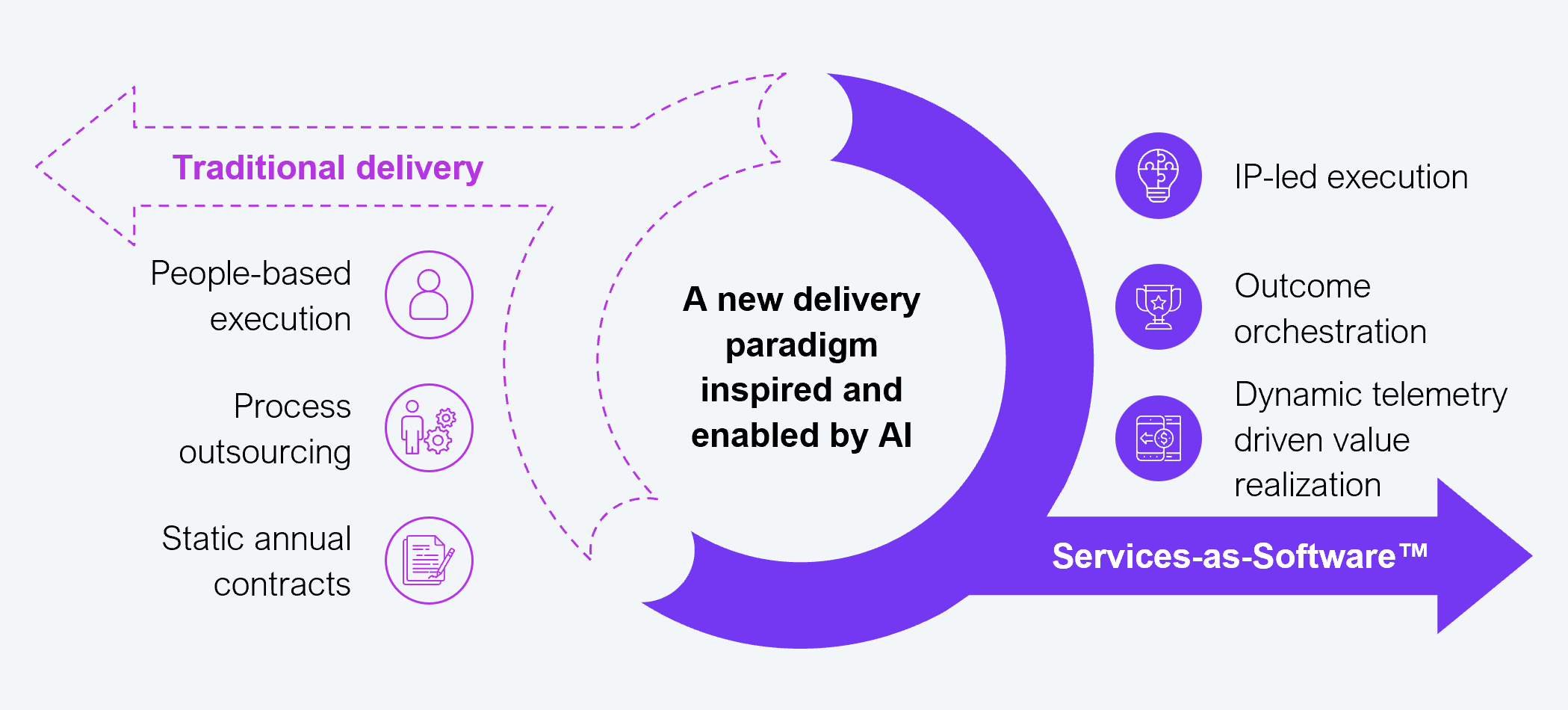
Source: HFS Research, 2026
For decades, technology operations leaders have attempted to migrate their legacy CAPS to modern systems with limited success. Often, they have ended up with more systems rather than fewer, as business complexity, customer obligations, and cost constraints limited complete systems migration. Now, in the age of AI, we not only have the benefit of technology but also that of a new delivery paradigm in Services-as-Software. It is a golden opportunity to overcome past challenges and be part of the solution with enterprise-wide impact.
Benefit 1: Rapid cost takeout
Benefit 2: Reduced operational risk
Benefit 3: Outcomes that matter
The bulk (50%–75%) of a CIO’s operating budget at an average-sized health plan (encompassing one to five million lives) is consumed by managing and maintaining multiple CAPS. The typical CAPS landscape includes mainframes, on-premises legacy systems, and some cloud-enabled modules. Adding to semi-integrated systems’ complexity is business complexity, with multiple service lines (employer, administrative services organization, Medicare, and Medicaid) and evolving business rules spread across CAPS. This complexity will continue to increase costs unless health plans embrace a radical new path, Services-as-Software.
The Services-as-Software delivery paradigm maximizes AI’s potential while laser-focusing on outcomes. Health plans, facing a rapidly shifting value proposition, must begin targeting what matters most: materially improved operational outcomes at lower cost, with warp speed.
Health plans are traditional outsourcing veterans, but traditional outsourcing won’t deliver exigent results. Health plan CIOs must collaborate with procurement leaders to embrace SaS-enabled sourcing.
The plan to outsource CAPS: Line-item capabilities must not constrain better outcomes
Contrary to popular narratives, CAPS are neither differentiators nor strategic assets, and they have not been for a long time. It is time to shift the approach to sourcing outcomes rather than traditional capabilities sourcing. However, given that CAPS capabilities are key to delivering services to members, supporting enterprise financials, and remaining compliant with regulations, sourcing execution must be strategic and practical.
Exhibit 2 provides a high-level roadmap and approach for transitioning from traditional delivery to AI-enabled Services-as-Software.
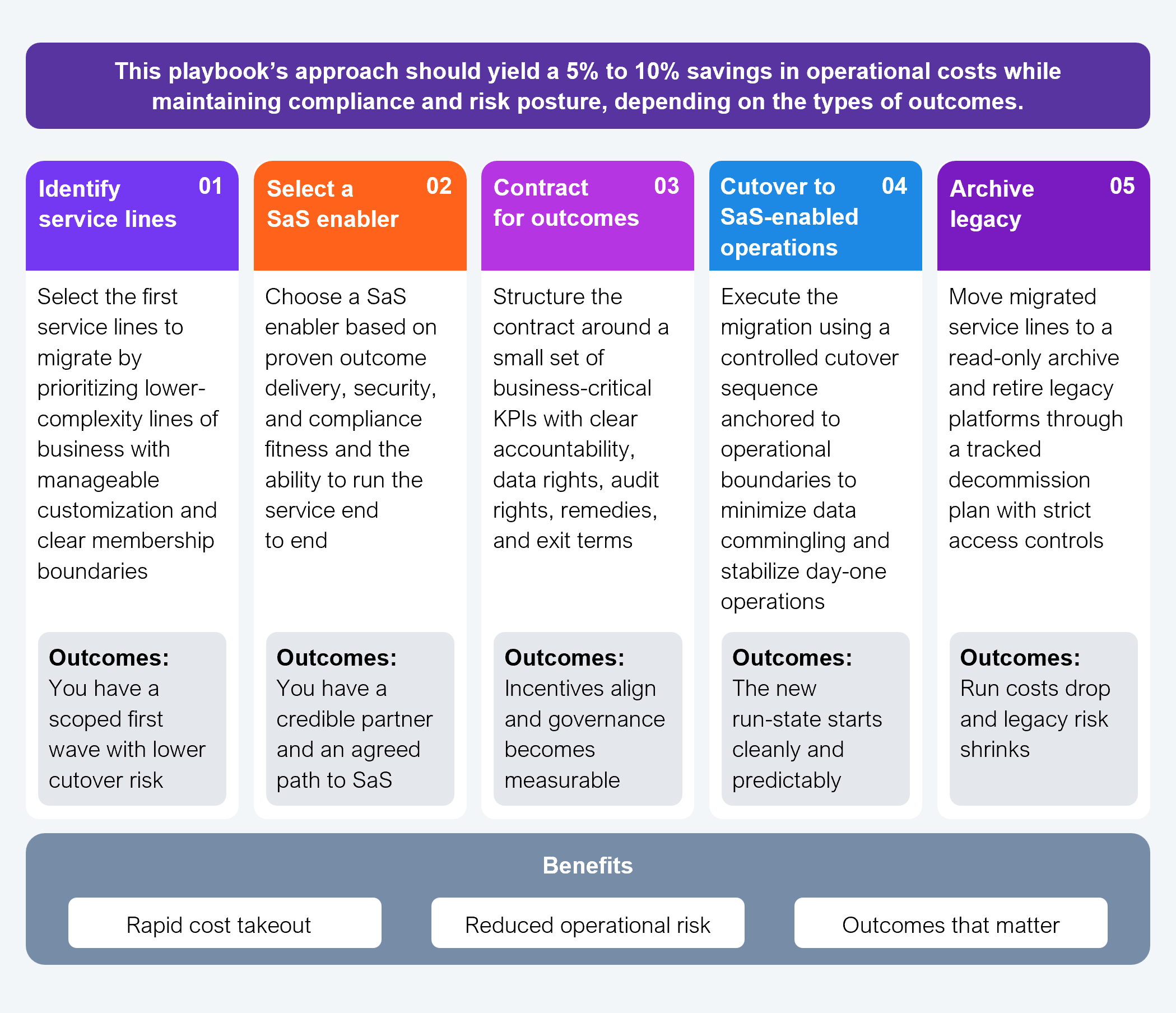
Source: HFS Research, 2026
Details matter when migrating operations to a new delivery paradigm. The summary in Exhibit 2 illustrates the journey ahead, but the playbook provides the execution details you’ll need for success.
Health plan CIOs cannot continue to maintain the status quo landscape of CAPS. There is no purpose to it anymore. The faster they exit CAPS, the greater the value they add to the health plan operations. This playbook provides a clear-eyed path to doing it by leveraging AI and a new delivery paradigm.
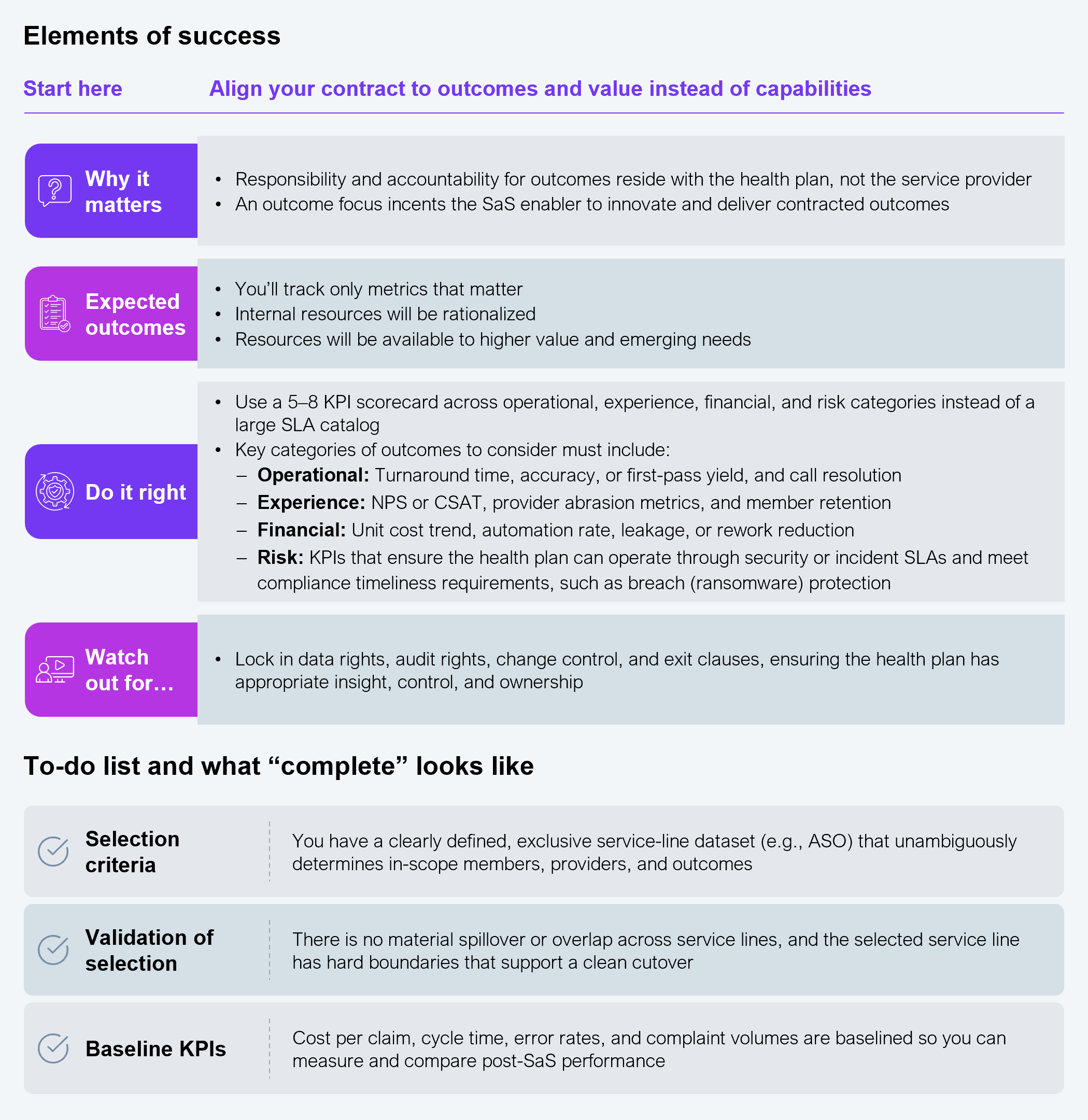
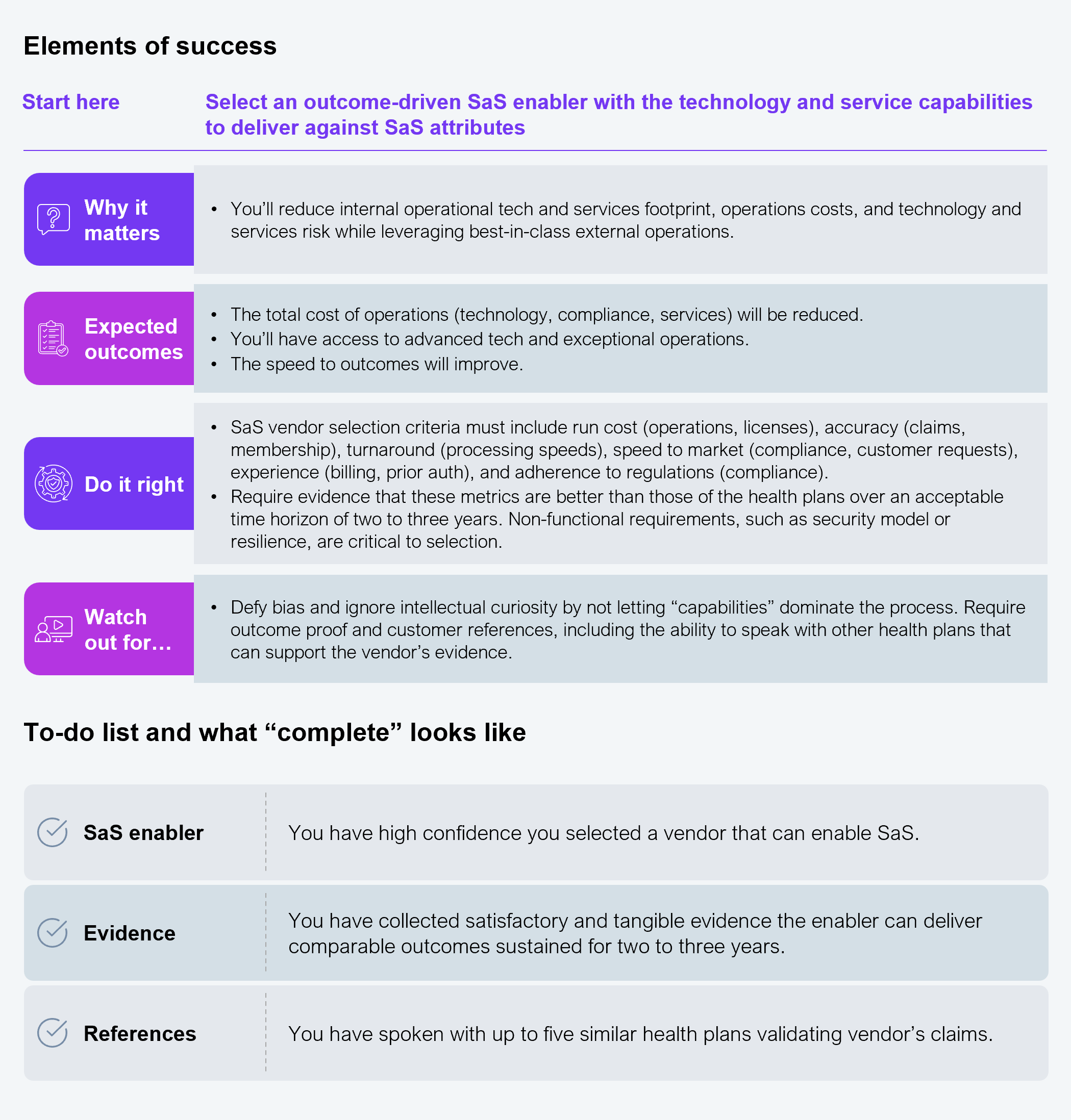
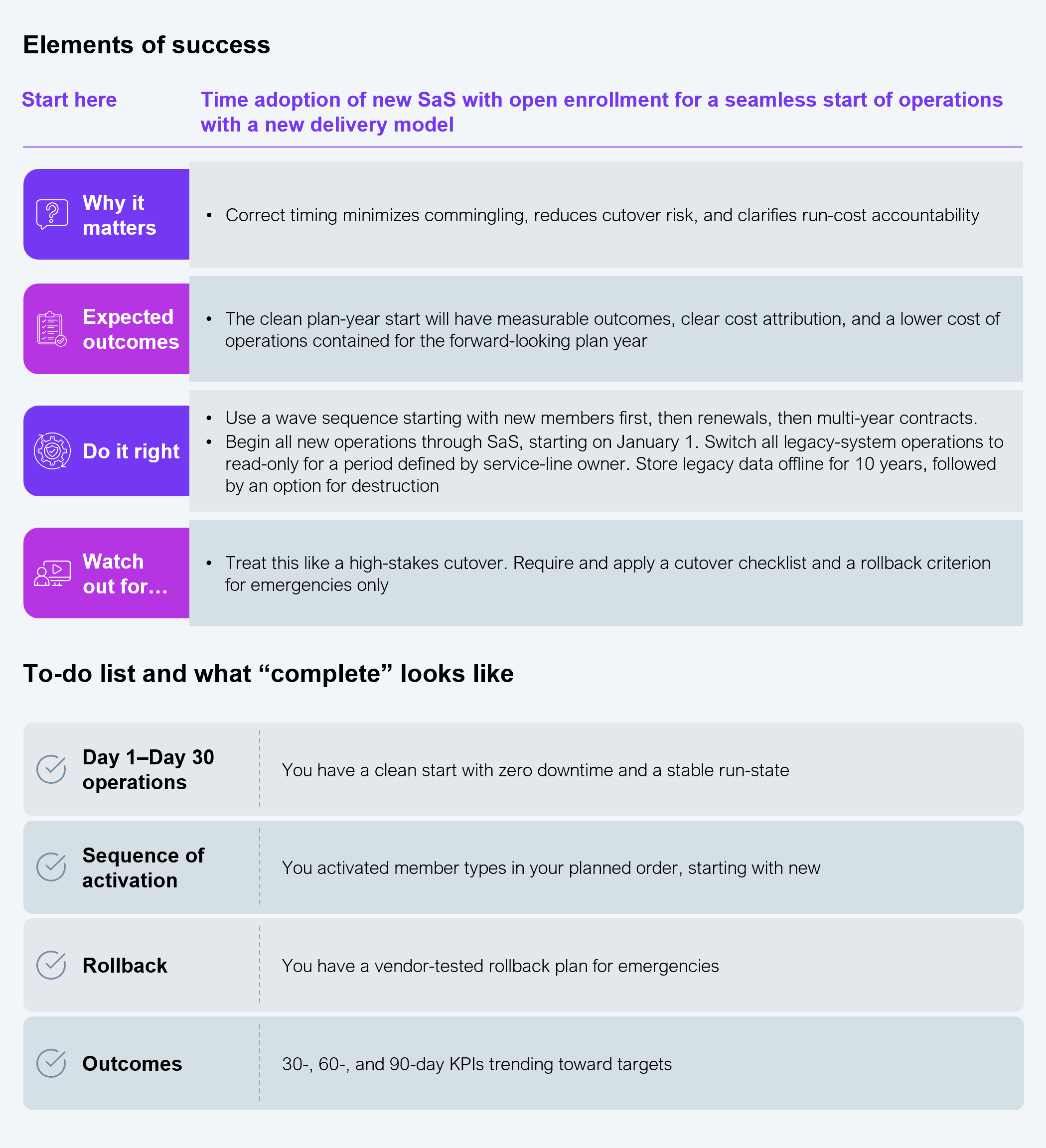
Health plan CIOs must avoid analysis paralysis by adopting the least-resistant path from start to finish (see Exhibit 3) to be ready for open enrollment and the beginning of the plan year.
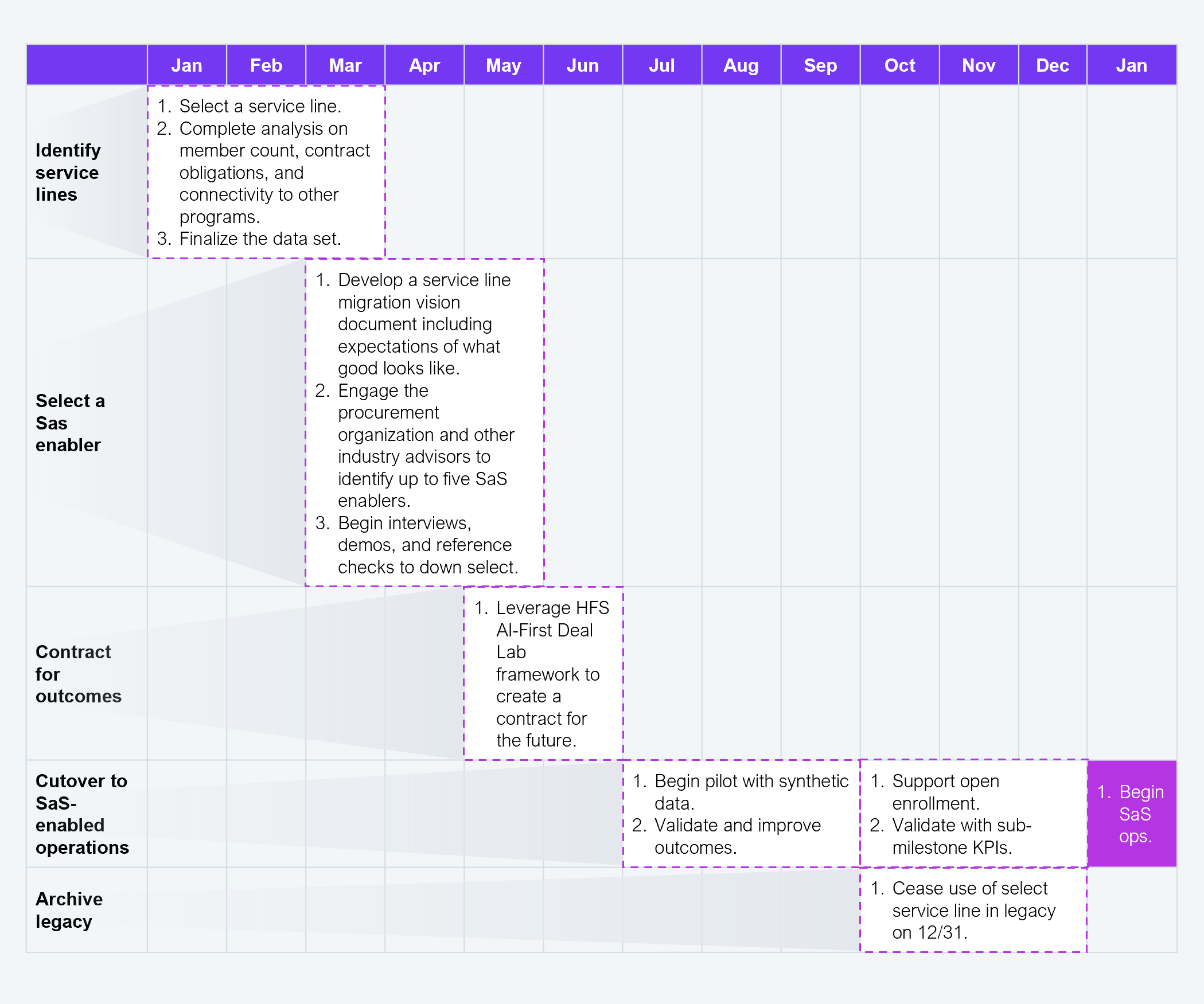
Source: HFS Research, 2026
Risk 1: Entrenched thinking and execution
Across industries, technology and operational leaders have leaned into what they know. While this approach may appear to mitigate the risks of the unknown, it would have missed the opportunity to adopt new ways to deliver higher value at lower cost.
Risk 2: Risk, compliance, and controls should be attached to outcomes
A health plan is responsible to regulators and customers. Consequently, contract outcomes must include a control set for audit rights, data ownership, incident SLAs, regulatory reporting responsibilities, and service credits tied to measurable KPIs.
Risk 3: Continuous improvement and outcomes validation
Complacency is often a by-product of outcome-based contracts, given that there are no operational or capability roles for the health plan. Drive continuous improvement of associated KPIs while validating the achieved outcomes. To ensure both tenets are completed, the contract must include financial and operational remediation and penalties.
The following list includes relevant HFS perspectives on health plan operations in a shifting market; watch for our series on executing Services-as-Software within a health plan and on selecting the right partner for success.
Register now for immediate access of HFS' research, data and forward looking trends.
Get StartedIf you don't have an account, Register here |
Register now for immediate access of HFS' research, data and forward looking trends.
Get Started