US healthcare will continue to face various challenges, including cost, epidemics, disease prevalence, access, clinician shortage, and an aging population, all of which will worsen as demand increases and supply shrinks. Agentic AI will have to play an oversized role in managing some of these challenges addressed in Part 1 of this series.
The US is currently short of 55,000 doctors and 79,000 nurses. That number will increase to about 80,000 for doctors and remain at a high of 65,000 for nurses. The confidence of those metrics is limited given the level of uncertainties in societies and their implications. To add a twist to the shortages, there is a gap between the type of clinician needed and the demand (see Exhibit 1), e.g., by 2034, there will be more older people than younger, yet the clinician specializations don’t align with the needs of the time. Given that graduating more doctors will not bridge the gap, the only real path to maximizing clinician time is delegating all administrative processes to agentic so clinicians can focus on delivering care and helping health systems and hospitals stay financially healthy.
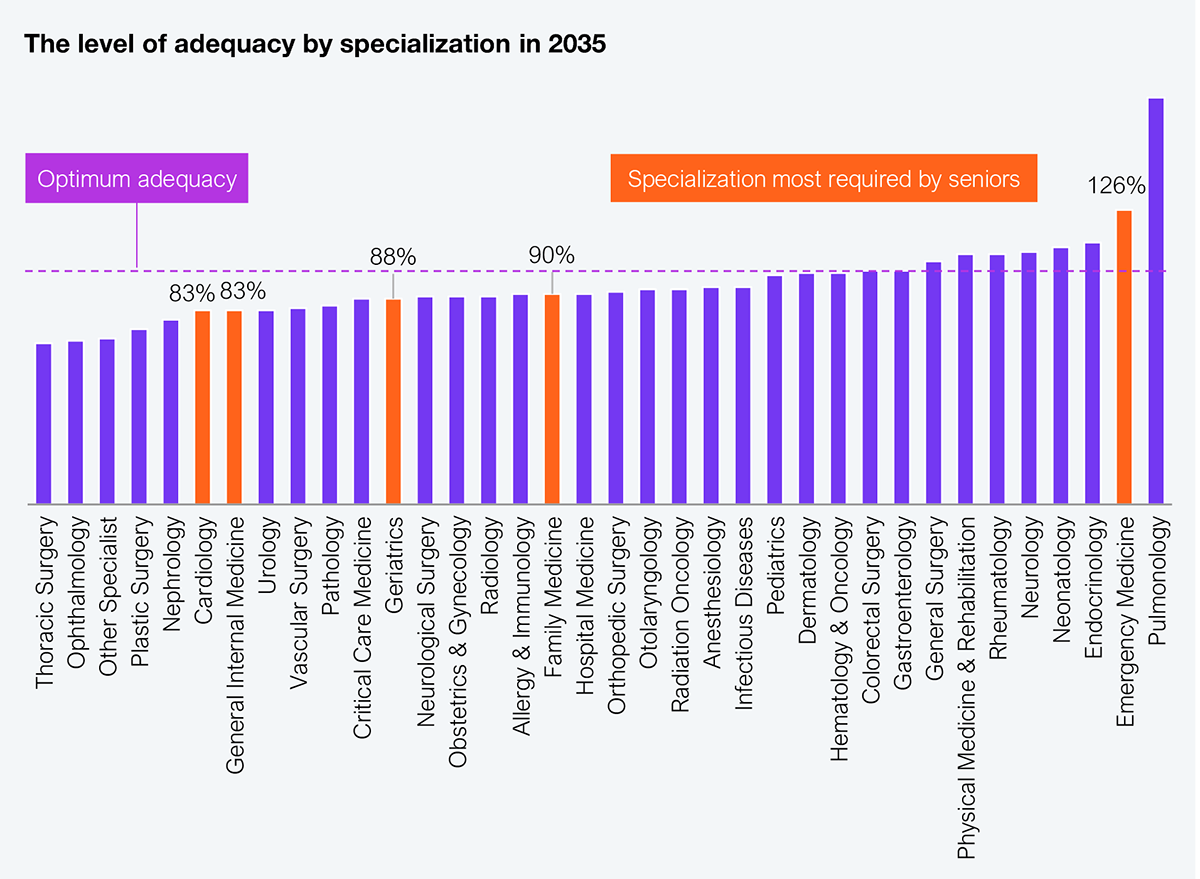
Source: Bureau of Health Workforce, US Dept. of Health and Human Services, HFS Research, 2025
Administrative processes forced upon doctors by health plans, such as prior authorizations (PA) and regulators for various reporting requirements, can be significant. Several estimates indicate that doctors spend between 20% and 35% of their time on non-clinical functions, including billing, insurance processes, and compliance documentation. Spending eight to 14 hours of a 40-hour week regularly on these functions is detrimental to doctors (loss in income, lower satisfaction, limited access to patients) and patients (increased costs, reduced access, delayed care). In a landscape of increasing demand and declining clinical supply, administrative burdens are corrosive and harmful to care delivery and hospital financials as they divert clinical time to unnecessary tasks.
While healthcare funders (payers, government) will always raise the bar for access to their funds, clinicians now have a new tool to fight this battle for them—agentic AI (see Exhibit 2). Task-based agentic is now commonplace for auto-generated clinical notes, detecting fraudulent claims, and managing prior authorizations. However, by 2027, we should expect multi-agentic (multiple specialized agents that collaborate to perform complex, interrelated tasks autonomously) to have a significant footprint.
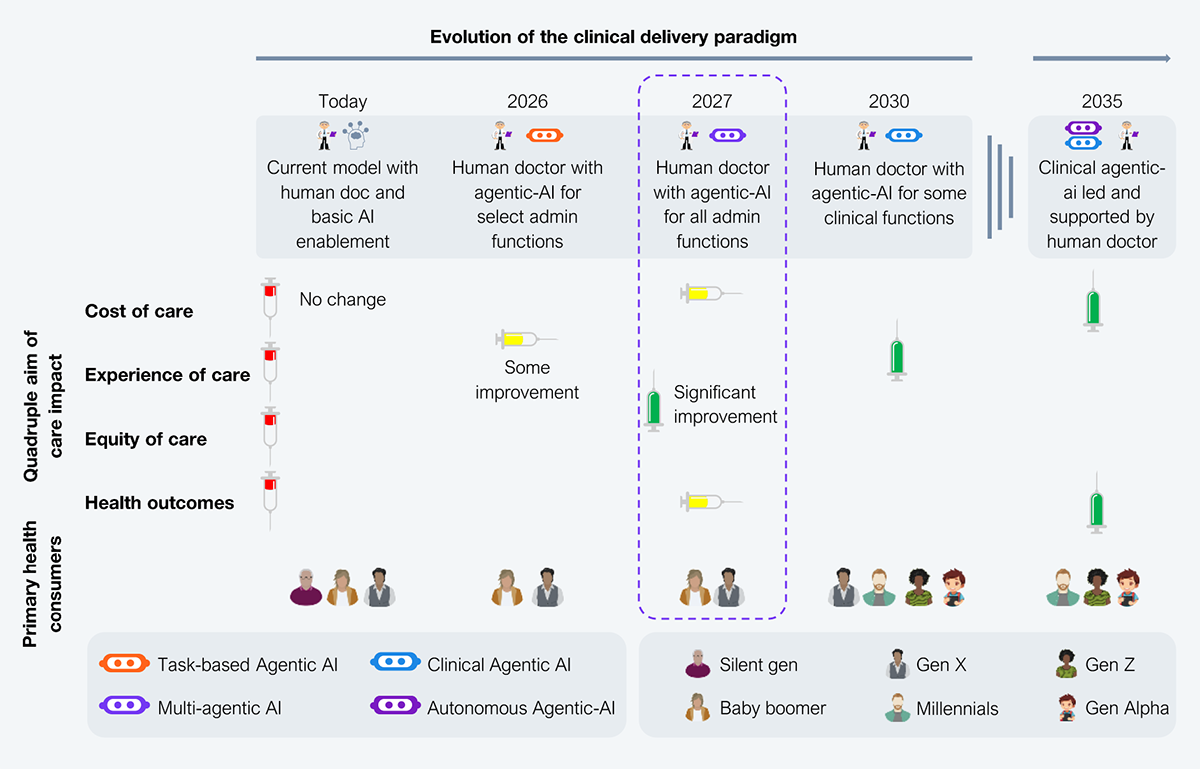
Source: HFS Research, 2025
Marketers have been very busy painting anything remotely AI as agentic. There is a clear technical difference between AI agents and agentic AI. The agentic architecture, orchestration, dynamic registry, and memory layer are some attributes that separate it from AI agents, aside from the outcomes. So, conducting deep diligence on any agentic AI solution is critical to validate its authenticity.
Yet some examples have a multi-agentic feel (see Exhibit 3). While the hype of AI is powerful, there are many questions to answer about the multi-agentic properties of solutions. Key filters for multi-agentic AI include system freedom to reorder tasks, backtrack, or invent new subtasks, continuous learning, context accumulation, avoidance of repeat work, support parallel, multi-modal, or multi-domain workflows without manual prompts.
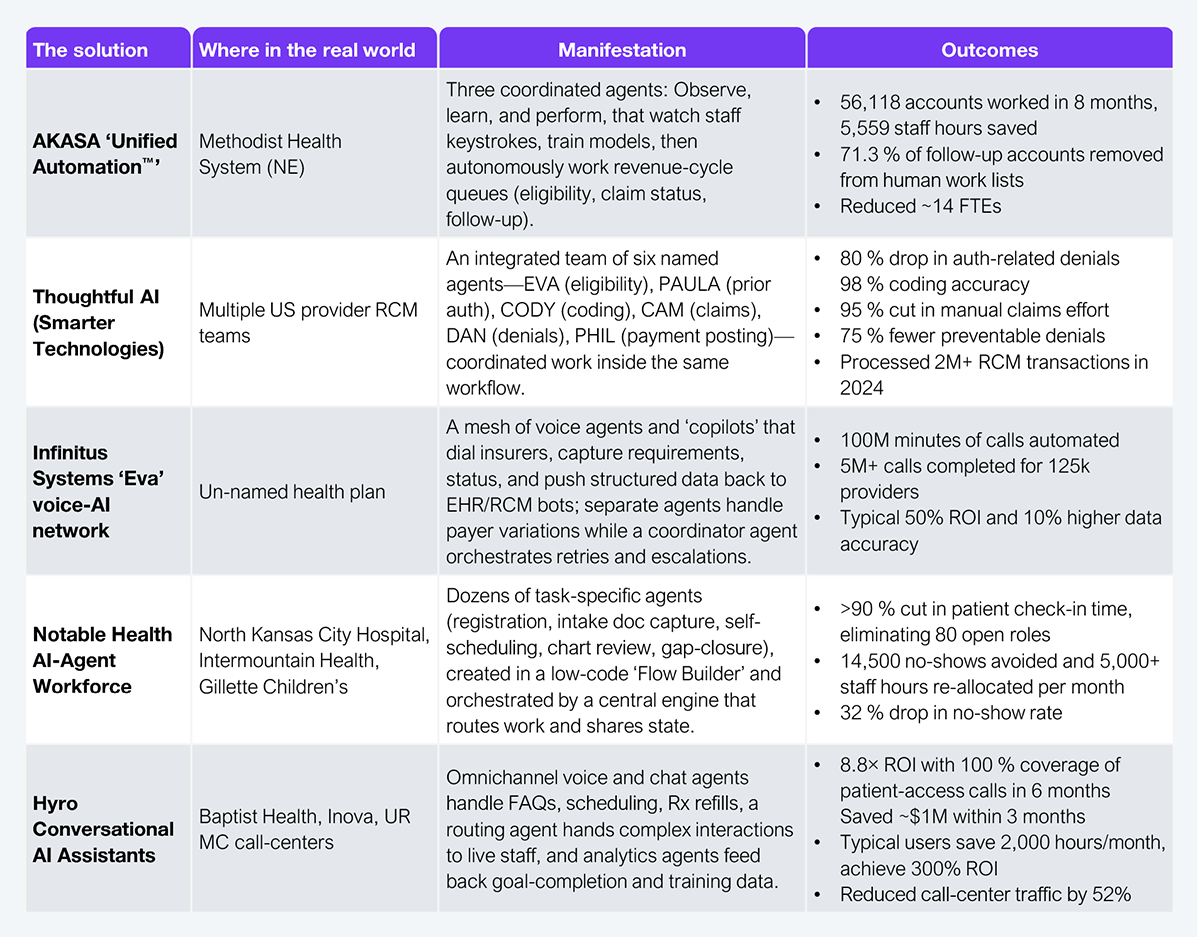
Source: HFS Research, 2025
The value of multi-agentic AI currently appears to be focused on addressing legacy challenges that are about increasing barriers to care (prior authorizations, appeals management), payments (claims, billing), and customer service to achieve cost savings by reducing headcount and completing processes faster, and by some measure, with greater levels of accuracy. While some legacy processes are deliberate, others, such as member services, can be proactively addressed. Most member service calls are to understand eligibility for benefits and the benefits in the plan. Similarly, patients in a post-acute setting need help to learn about support resources or clarification of medications. All of these can be addressed proactively and consistently with multi-agentic AI connecting earlier and often with members and patients through the channels of their choice and supporting their needs. Health plans and health systems have an opportunity to truly open their minds to the possibilities.
Like all new technologies, AI poses various risks that can fuel pessimism about its potential. Understanding those risks and developing specific remedies is essential to ensuring deliberate and timely actions. While the challenges may seem daunting, the end goal of maximizing clinician time is a huge prize for both health systems and society in general.
Clinician retirements, early exits due to burnout, and medical graduate output not meeting population demands are driving the depressed clinician count for the next decade and possibly beyond. Technology is the only way to bridge the gap between supply and demand. Agentic AI is promising enough to invest in and embrace sooner rather than later to strengthen hospital financials.
Register now for immediate access of HFS' research, data and forward looking trends.
Get StartedIf you don't have an account, Register here |
Register now for immediate access of HFS' research, data and forward looking trends.
Get Started