Health systems and hospitals are slowly but increasingly exploring the use of agentic AI in clinical settings. While the rationale is urgent (cost, clinician shortage, access), it also signals the evolution and confidence beyond the use of agentic AI to address the administrative processes discussed parts 1 and 2 of this series.
Clinical agentic can and is beginning to improve health outcomes, reduce clinical inefficiencies, and bridge the clinician shortage gaps based on real-world examples. Health system and hospital system leaders who are sitting on the fence or resisting the adoption of agentic AI in the clinical workflows will experience declining revenues, poor health outcomes, and reputational damage. Adopting clinical agentic is thus not optional; it is mandatory to survive and realize the value proposition of care delivery.
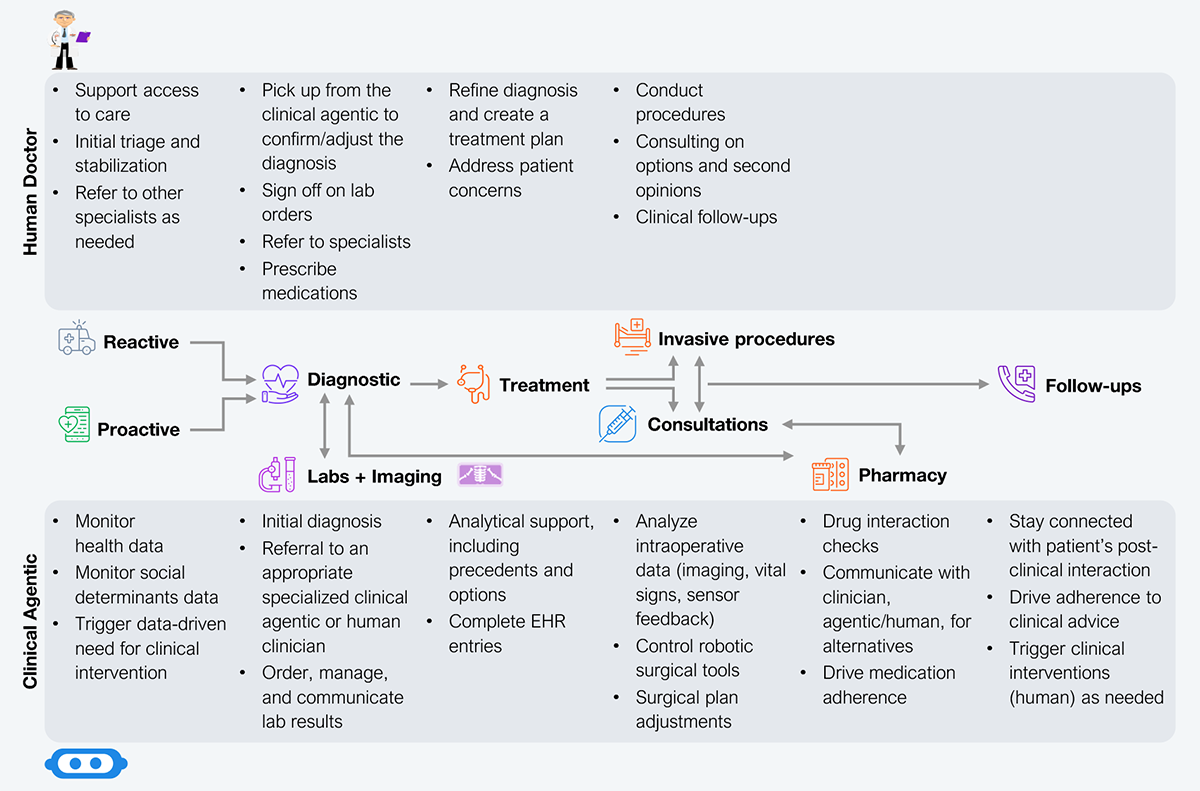
Despite the clinical supply challenges plaguing the world as it gets older and sicker, we are nowhere near replacing the human doctor or nurse with AI. However, agentic AI is now augmenting their roles to optimize the clinical time available. Exhibit 1 illustrates the roles of the human doctor and clinical agentic across a patient’s care journey—balance clinical risk (regulatory compliance, protocol adherence), improve patient access (addressing equity, clinical footprint), and consistently deliver the best health outcomes (clinical decisioning, focus on quality).
Source: HFS Research, 2025
The human clinician’s role will largely be the same in the next five to ten years. To remain compliant with regulations, clinicians will still have to provide physical aid, conduct surgical procedures, write prescriptions, and sign off on all order types. However, they will have a greater level of freedom to practice the real art of treating patients and curing diseases.
A key enabler driver of this freedom will be clinical agents taking on larger routine burdens across the patient journey (see Exhibit 1). They can initiate diagnosis to route patients to the right clinicians, manage lab and imaging orders (including reading and interpreting the results), ensure accurate and up-to-date EHR entries, conduct drug interaction checks, recommend alternate medications, and handle all post-care follow-up to drive patient adherence to clinical orders. This will return highly monetizable time to clinicians while driving consistent care, resulting in better health outcomes.
Furthermore, clinical agentic can drive the health journey (need-based care paradigm) by monitoring a suite of health, healthcare, ambient, and other ancillary devices in a home environment—layering it with the individual’s social determinants of health—and managing their health outcome, including triggering clinical interventions on a need basis. The ability to trigger interventions helps optimize human clinician time only when necessary, such as for cost reduction, and improve health outcomes by ensuring proper care at the right time.
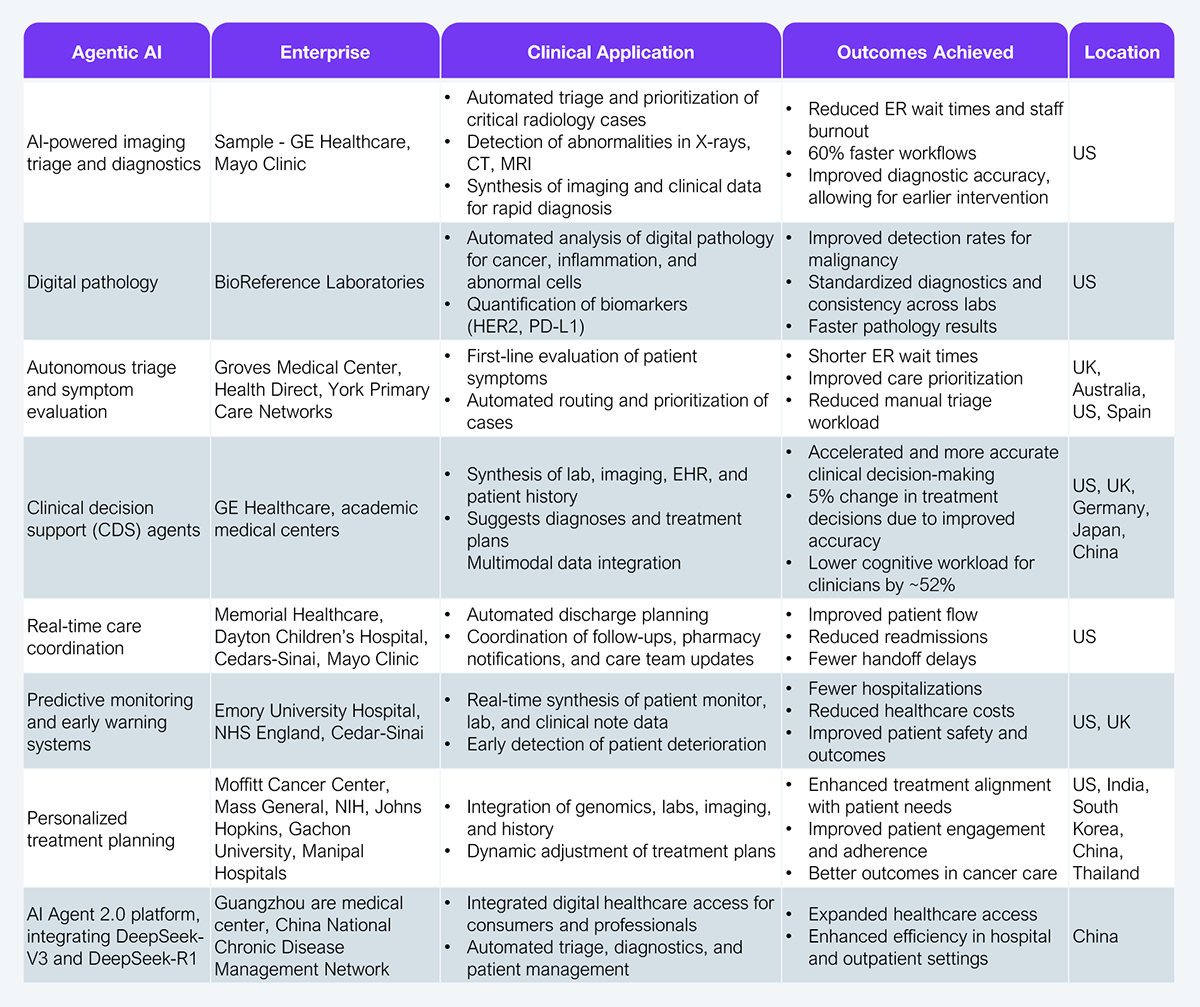
Agentic AI is real in clinical settings (see Exhibit 2) as it is increasingly deployed worldwide and across the patient care journey. Its adoption—from triaging and clinical decision-making to early warning and personalized treatment planning—indicates the increased faith that health systems and hospitals have in the technology. That is bolstered by the outcomes achieved, particularly in improving hospital financials (reduced ER admissions, improved patient throughput, better clinician burnout management) and health outcomes (diagnostic accuracy, speed to interventions, improved patient safety).
Source: HFS Research, 2025
The fact that big-name health systems such as Mayo Clinic, Johns Hopkins, and Cedars-Sinai in the US, the NHS in England, and multiple systems in China have adopted agentic AI in clinical settings indicates there is buy-in by both clinicians and administrators. While these deployments are not at scale or the first stop for patients, they are actively being integrated into clinical workflows. So the longer they stay and continue to improve, the greater the likelihood that agentic AI will expand its value proposition and influence across the patient care journey.
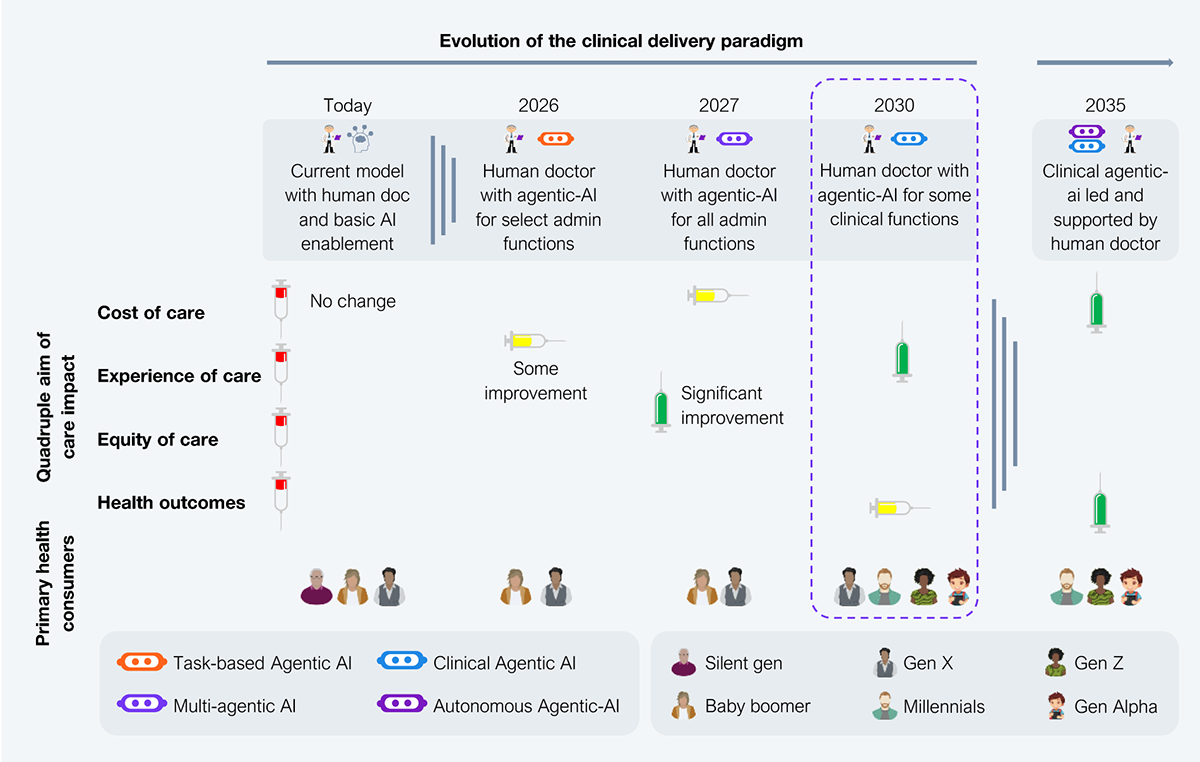
Agentic AI in healthcare (see Exhibit 3) is making its way from addressing the low-hanging fruit of inefficient administrative processes as a single function (task-based) to automating and orchestrating complex administrative processes through multi-functional agentic AI between now and 2027 (potentially accelerating with increased adoption as models improve). While the traditional approach starts with low-risk activities and delivers meaningful benefits before moving to more complex activities, healthcare may be disrupting that to some extent (covered in earlier parts). Increased enthusiasm and associated real-world deployments across task-based, multi-agentic, and clinical agentic could disrupt the linear roadmap (see Exhibit 3), with parallel growth of clinical agentic possibly reaching scale well before the 2030 estimate if current experimentations render successful results by 2027.
Source: HFS Research, 2025
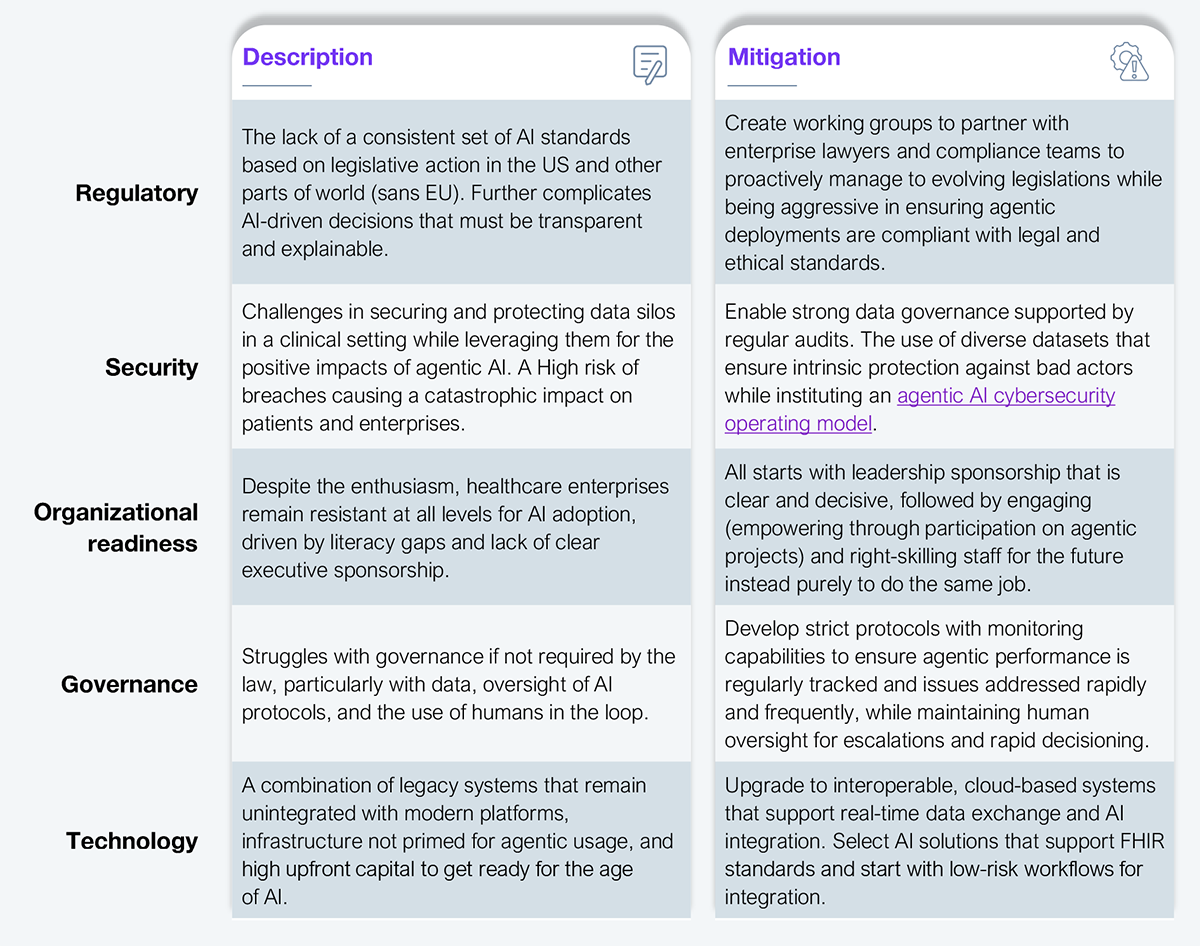
Despite the advancements in agentic AI, billions in investments, and the enthusiastic adoption by multiple health systems and hospitals worldwide, we are not yet ready to declare victory. Many challenges (see Exhibit 4) must be addressed before progress at scale can be considered sustainable.
Source: HFS Research, 2025
The drivers (cost, clinician shortages, disease prevalence, aging) for agentic AI in clinical settings are real and present. They are not going anywhere, not for the foreseeable future. However, they must be addressed to support the next few generations.
Register now for immediate access of HFS' research, data and forward looking trends.
Get StartedIf you don't have an account, Register here |
Register now for immediate access of HFS' research, data and forward looking trends.
Get Started