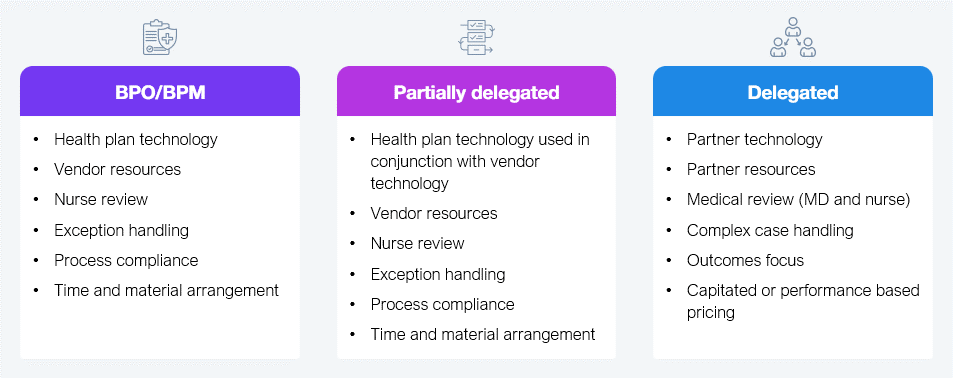
Utilization management (UM) helps health plans decide if a medical service is necessary before they agree to pay for care. It has been evolving over time to reduce cost, improve efficiency, and, according to some, improve health outcomes. WNS HealthHelp has been pushing the boundaries for innovation in this space with its platform CONSULTTM, providing augmented support across several clinical areas. WNS HealthHelp incorporates practicing physicians and their real-world expertise across all clinical domains, including the cardiology, musculoskeletal, oncology, radiology, and sleep therapy domains, delivering healthy outcomes while being flexible (see Exhibit 1) in engaging with health plans.
Source: HFS Research, 2025
The acceleration of electronic health record (EHR) systems due to Meaningful Use regulations changed how UM was conducted—going from a manual, inconsistent, and lengthy cycle time to a greater level of automation that rendered highly consistent evaluations.
However, as cost of care escalated—due to increased demand driven by expanded access, disease prevalence, and the influence of pharmacy benefit managers (PBM)—UM had to evolve. It now addresses the volume of requests, speed to evaluation, and the need to incorporate an extensive range of medical literature into decisioning.
The new UM solution comes at time when authorization requirements have risen sharply. Health plan benefits increasingly need prior authorizations before treatment is given. The number of prior authorizations (PA) more than tripled from 2005 to 2023 (an estimated 50 million PAs processed just for Medicare in 2023 alone).
Moreover, slow UM and delayed PA have led to treatment delays, a higher propensity for adverse events, and more consumers abandoning medical care. As a result, AI is being leveraged to play a critical role—make UM faster, consistent, less expensive, and better equipped to reduce fraud, waste, and abuse.
There are several big-league options in the market, including Carelon, EviCore, and Evolent. These companies claim to work against the grain to improve traditional UM, but the results are patchy at best.
WNS HealthHelp is embracing the possibilities of AI to tackle the endemic challenges of UM and PA, particularly the inefficiencies and delays in seeking approval for diagnostic imaging and other medical services. CONSULTTM streamlines processes by integrating AI and automated workflows that accelerate and improve the accuracy of medical necessity determinations. By leveraging generative AI technology, WNS HealthHelp incorporates virtual clinical agents to improve speed, accuracy, and ultimately quality by allowing clinicians to focus on the most challenging cases.
WNS HealthHelp’s approach to addressing the UM/PA space through CONSULTTM. has three key attributes:
WNS HealthHelp’s CONSULTTM has delivered tangible outcomes for providers, patients, and their health plan clients on key performance metrics such as experience, turnaround times, and denial rates. Some notable impacts are:
WNS HealthHelp claimed a strong 70% reduction in decision time among other impacts, health plans must weigh the metrics against potential regulatory hurdles and provider pushback. They should also scrutinize how the platform integrates with their existing EHRs and legacy UM processes. Is WNS HealthHelp truly interoperable, or does it require expensive and time-consuming integrations that dilute ROI? Legacy UM needs a shake, and WNS HealthHelp is a viable option.
Register now for immediate access of HFS' research, data and forward looking trends.
Get StartedIf you don't have an account, Register here |
Register now for immediate access of HFS' research, data and forward looking trends.
Get Started