Policymakers and healthcare executives have long been obsessed with governance models (centralized, decentralized, or hybrid), believing that structural elegance can produce better health outcomes. While there is no evidence that any model works consistently, this structural fixation distracts from the core issue of ‘health’—shaped by social, economic, and environmental conditions, not governance models. To realize meaningful returns on healthcare investments, enterprises must focus on the social determinants of health (SDOH) regardless of the governance models.
Shift enterprise healthcare spending from reactive care to proactive health investment
The most decisive interventions in global health didn’t begin in government offices or hospital boards. They started in schools, farms, homes, and local neighbourhoods. Let’s stop confusing centralized consistency with success and decentralized agility with access. Neither works if the system is blind to the root cause of illness. Enterprises must understand that spending on prevention is far more cost-effective than funding reactive clinical care (see Exhibit 1).
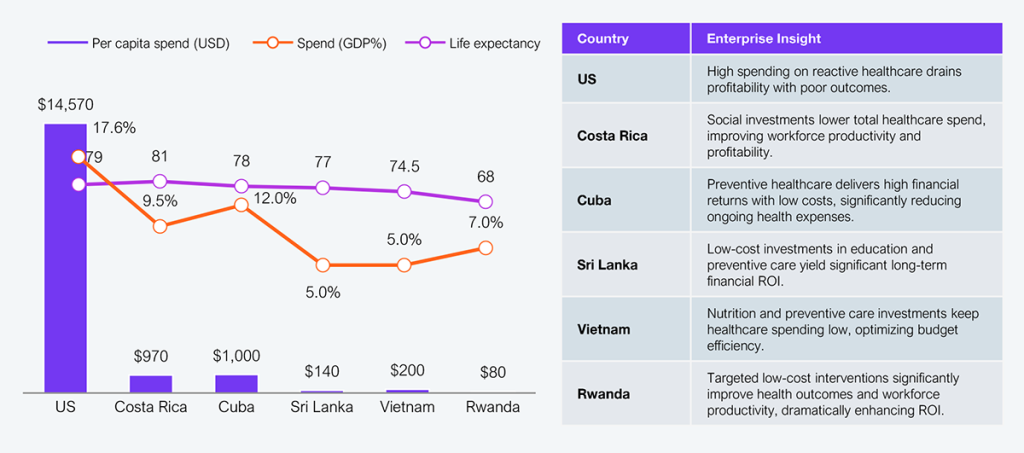
Exhibit 1: High spend does not ensure better outcomes; social investments can drive global health success
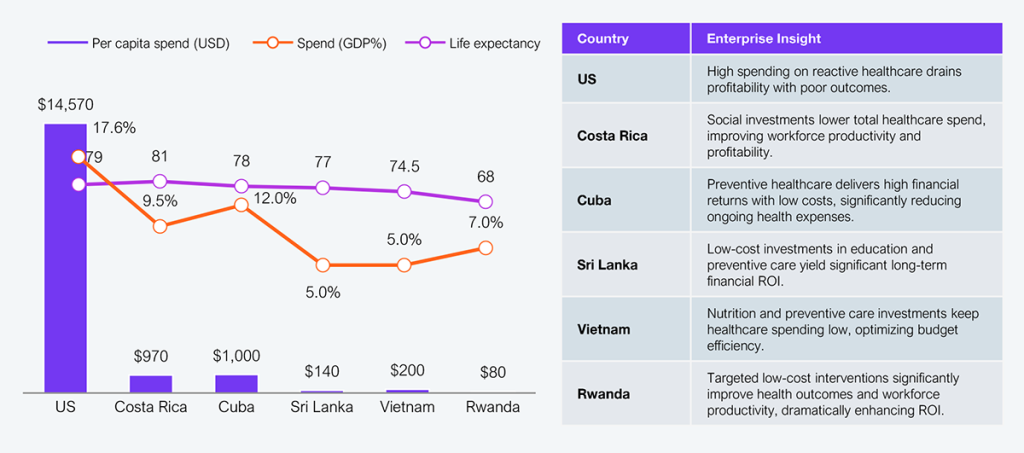
Note: Data is based on secondary sources and may vary by source and year. Accuracy is intended but not guaranteed. For comparison, a 2023 baseline is used where possible; where unavailable, earlier data was approximated and more recent figures may exist.
Source: WHO Global Health Expenditure Database, World Bank, Our World in Data, Macrotrends, HFS Research, 2025
Spending more does not mean better outcomes. Investing strategically in SDOH provides significantly better returns, enhancing societal outcomes and enterprise sustainability.
Spending on prevention reduces longer-term costs
Investing upstream significantly reduces future healthcare spending by preventing chronic conditions, cutting back acute care costs, improving workforce productivity, and enhancing brand reputation and market positioning. We see proof, from Latin America to Africa and Southeast Asia, that such investments in social conditions yield exponential returns:
Educated communities mean healthier, more resilient workforces
- Sri Lanka reduced maternal mortality from ~600 to just 60 per 100,000 live births by embedding universal female education, boosting literacy above 90%, and deploying public health midwives into rural communities to provide antenatal care, birth support, and follow-ups.
- Ethiopia halved the proportion of women without education between 2000 and 2019, enabling better health-seeking behaviour. Increased access to literacy bumped up antenatal visits and faclity-based care, directly improving maternal and newborn survival rates across thousands of underserved villages.
Takeaway: Support health interventions driven by education through CSR, funding models, or ecosystem partnerships. Integrate maternal education into digital health platforms and outreach. Funding initiatives focused on education-driven health directly reduce future clinical costs, enhance workforce productivity, and ensure sustainable profit margins.
Behavioural incentives reduce clinical risk and workforce churn
- Brazil: The Bolsa Família program tied cash assistance to school attendance and child health checkups. In poor municipalities, especially among Black families, the child mortality rate fell. When integrated with Brazil’s Family Health Strategy, outcomes improved further—showing the power of combining incentives with primary care access.
- Mexico: Oportunidades (formerly Progresa), Mexico’s conditional cash transfer program, mandated school attendance and health visits—leading to increased childhood immunizations, improved nutrition, and reduced anemia. Children from participating households had better health metrics and school completion rates, breaking cycles of intergenerational poverty.
Takeaway: Creating incentives focused on health behaviors reduces costly clinical episodes, driving profitability through lower healthcare spending and improved workforce performance.
Infrastructure first, tech later
- Costa Rica’s nearly universal access to clean water (98%) and sanitation (95%) played a decisive role in slashing infectious disease rates. This investment in core infrastructure, rather than high-tech interventions, drove superior child health outcomes and supported the country’s impressive life expectancy of ~81 years.
- Vietnam cut child stunting to under 20% through aggressive nutrition programs, early-life interventions, and near-universal vaccination coverage. By investing in basic needs—sanitation, food security, and preventive care the country achieved life expectancy levels comparable to wealthier nations at a fraction of the cost.
- Cuba’s public health model includes a robust immunization campaign and a strong nutrition support system. These efforts have eliminated many vaccine-preventable diseases and drastically reduced malnutrition, resulting in one of the lowest infant mortality rates in the developing world despite constrained resources and economic sanctions.
Takeaway: Explicit infrastructure investments deliver rapid, measurable financial returns by significantly reducing costly healthcare episodes and boosting workforce productivity.
Primary care as a community anchor
- Cuba’s 20,000 consultorios each pair a physician with a nurse for conducting home visits, tracking family health histories, and making annual community health assessments. This highly localized, prevention-first system consistently delivers outcomes, especially infant survival and chronic disease control, rivaling those of high-income countries.
- Brazil’s Family Health Strategy deploys multidisciplinary teams comprising doctors, nurses, and community agents to provide proactive, relationship-based care in underserved areas. Infant mortality dropped 25%, showcasing the superior impact of decentralized, locally rooted primary care.
- Ethiopia’s Health Extension Program trained and deployed more than 40,000 workers in villages. These workers deliver maternal care, sanitation guidance, and immunizations, bringing care to the doorstep. The result: improved health literacy, reduced preventable deaths, and a notable increase in maternal and child survival.
Takeaway: Shift investments directly to primary and community-based care models to substantially reduce healthcare expenditures, increase productivity, and optimize financial outcomes.
Community-led programs deliver enterprise-grade results
- Rwanda has more than 45,000 volunteer community health workers to provide basic care, track population health data, and deliver education across rural and urban areas. Their integration into the national system, backed by performance incentives, has strengthened trust, improved disease surveillance, and driven measurable health gains since 2000.
- Costa Rica’s approach to combat Chagas disease involved the collaborative efforts of health/housing ministries and residents to improve home construction and educate families on vector risks. This locally driven initiative improved disease control by aligning public infrastructure, civic participation, and household behaviour change.
Takeaway: Direct enterprise funding for community-led programs reduces healthcare spending and enhances workforce performance, driving measurable profitability improvements.
Build health ecosystems around outcomes, not org charts
The future focuses on orchestration, not centralization or decentralization. It emphasizes aligning actors, data, and funding around SDOH as the system’s core purpose, rather than treating it as a policy afterthought.
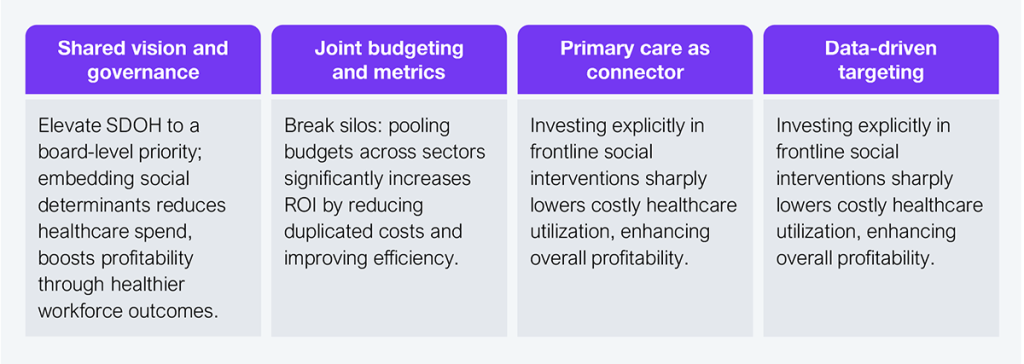
Exhibit 2: HFS’s four pillars of orchestrated health
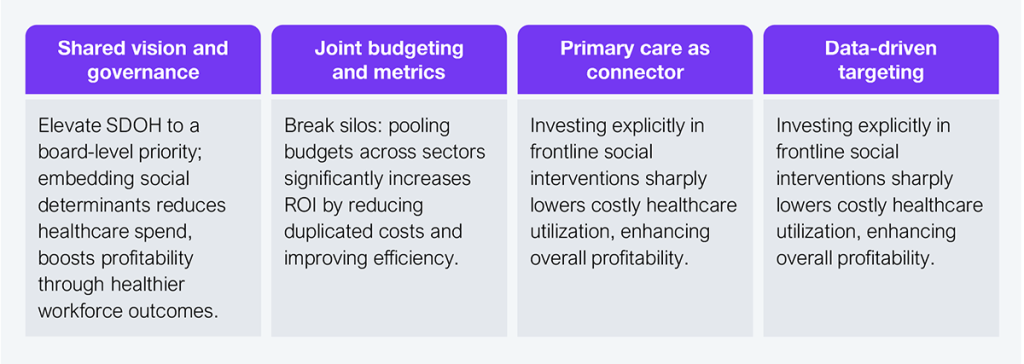
Source: HFS Research, 2025
The Bottom Line: Structural debates waste time. Focus on what drives social ROI to improve your financials.
Healthcare systems don’t collapse from structural flaws. They fail because they’re rigid, reactive, and blind to social realities. Enterprise leaders should keep the following in mind:
- Fund measurable, upstream social interventions: Proactively investing in education, nutrition, sanitation, and preventive care significantly reduces downstream healthcare spending. Enterprises that include social ROI in their healthcare budgets consistently see decreased chronic illness prevalence, lower acute-care utilization, and higher cost efficiency.
- Integrate social determinants into your analytics and health platforms: A targeted, preventative approach lowers operational costs, improves care management efficiency, and yields direct financial returns through reduced healthcare expenditures and improved patient outcomes.
- Build local partnerships and community-driven programs: Engaging directly with communities improves health outcomes from the ground up, enhances workforce productivity, reduces absenteeism, and creates significant reputational and market advantages. Enterprises that invest locally strengthen their market positioning, foster employee and consumer loyalty, and ultimately drive long-term profitability.